Bridging the Gap: A Strategic Approach to CME Needs Assessments
By: Alejandra Viviescas, PhD
In Continuing Medical Education (CME), a well-crafted needs assessment is more than a funding requirement — it’s the foundation of meaningful, measurable learning. Done well, it connects clinical realities to educational solutions, helping providers design activities that close gaps, improve care, and meet accreditation standards.
Since specializing in CME writing in 2024, I’ve developed needs assessments across a range of therapeutic areas. Each project has sharpened my approach and deepened my understanding of what makes a needs assessment not only informative, but persuasive. Through that experience, I’ve built a structured process that enables me to consistently deliver strategic, evidence-based work aligned with client goals.
In the sections that follow, I walk through this process — from the initial kick-off call to the final educational agenda — to illustrate how a thoughtful, structured approach can elevate the quality of CME content and support stronger proposals and educational outcomes.
1. Setting the Foundation with the Kick-Off Call
Even when provided with a detailed project brief, I always begin with a kick-off call. This conversation is about more than logistics — it’s where strategy begins.
During the call, I aim to clarify:
- Whether the needs assessment is in response to an RFP or unsolicited. This shapes how we frame the narrative, particularly in terms of urgency and alignment with sponsor priorities.
- Who the potential sponsor is. While the writing remains unbiased, understanding the sponsor helps define the disease state or clinical focus. A proposal that’s too broad risks missing the mark.
- Timeline and process. I confirm whether an outline is required, whether subject matter experts (SMEs) will be involved, and workflow details.
- The intended educational activity. Understanding the planned format and objectives helps me ensure that the identified gaps can realistically be addressed through the proposed intervention.
This shared understanding allows me to serve not just as a writer, but as a collaborative partner with strategic insight into the broader educational plan.
2. Understanding the Therapeutic Landscape
After clarifying the goals of the project, I turn to the clinical background. My aim is to understand the state of the field, not just what the guidelines say.
This includes:
- Reviewing treatment guidelines and clinical trial data
- Exploring how real-world practice diverges from ideal care
- Assessing where the field is evolving and what that means for learners
At this stage, I assess how the emerging insights correspond to Moore’s Levels of Outcomes. For example:
- A new treatment just entering the market may reveal knowledge gaps (Level 3).
- An established therapy that remains underused could signal competence or performance gaps (Levels 4–5).
Understanding the therapeutic landscape informs not just the content, but the type of education that will be most impactful.
3. Research with Intention: How I Build a Targeted, Evidence-Based Foundation
Every needs assessment begins with questions. What’s the state of care? Where are the disconnects? What do clinicians need to know, believe, or do differently to close the gap? I rely on a sound research process to move from early assumptions to evidence-based answers — and to begin shaping the story that the needs assessment will tell.
My research process is layered. It starts broad and becomes increasingly focused as the narrative takes shape. I begin by using AI tools like Perplexity and ChatGPT to generate a high-level overview of the disease state and identify preliminary gaps in care. This early scan gives me a rough framework and direction for deeper investigation. From there, I turn to clinical guidelines to define the expected standard of care and highlight areas where changes or controversies exist. I then review peer-reviewed literature through targeted searches on PubMed and Google Scholar, focusing on recent studies, therapeutic developments, and real-world challenges. Medical news outlets and expert commentaries provide additional insight into how clinicians are reacting to emerging data, while patient advocacy websites offer a valuable lens into unmet needs from the patient perspective. I compile all relevant sources in a structured spreadsheet, tagged by topic and relevance. From there, I filter and prioritize the materials that best support the narrative I’m building.
But the value of research doesn’t lie in volume. It lies in selectivity — choosing the right sources to build a cohesive, compelling, and evidence-based argument for education. Here are the types of materials I rely on most often:
- Review articles, for clinical context and to surface unresolved questions that point to persistent challenges
- Clinical guidelines, as a benchmark for expected practice and a touchstone for evaluating real-world alignment
- Clinical trials and FDA approvals, to highlight how new therapies are reshaping treatment standards
- Commentaries, interviews, and podcasts, for expert insight and narrative detail that brings the content to life
- Qualitative studies and stakeholder surveys, to reveal real-world behaviors, perceptions, and barriers
CME outcomes data, to validate the presence of a gap and demonstrate that education can effectively address it
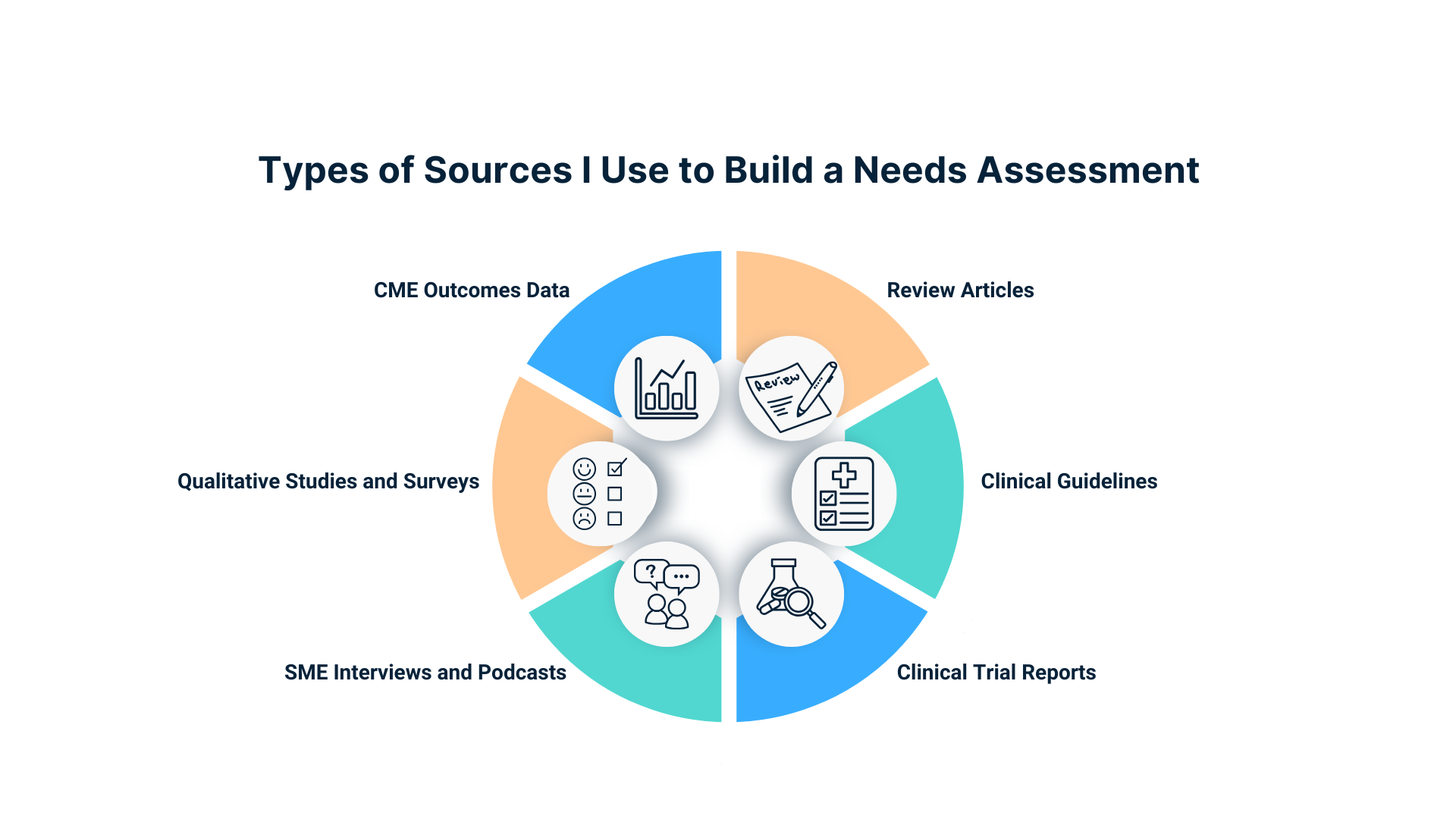
By grounding my needs assessments in research that is both rigorous and relevant, I ensure they clearly demonstrate the need for education and make a compelling case for the proposed activity.
4. From Structure to Story: How I Build Each Gap in the Needs Assessment
Once the research is complete, I begin shaping the narrative — and for me, that starts with structure.
Each gap in a needs assessment must do more than describe a problem; it must present a clear, evidence-based rationale for education and help define the type of intervention required To ensure this, I use a consistent five-part framework when writing my gaps:
- Expected Practice – What should clinicians be doing, according to current guidelines or expert consensus?
- The Challenge – What is preventing that practice from happening in real-world clinical practice?
- Supporting Evidence – What data, perspectives, or patterns demonstrate that the gap is both real and significant?
- Educational Need – What kind of intervention is required: knowledge-building, skill development, confidence-building, or behavior change?
- Outcomes Data – Where available, I include results from prior CME activities to show that similar education has made a measurable difference.
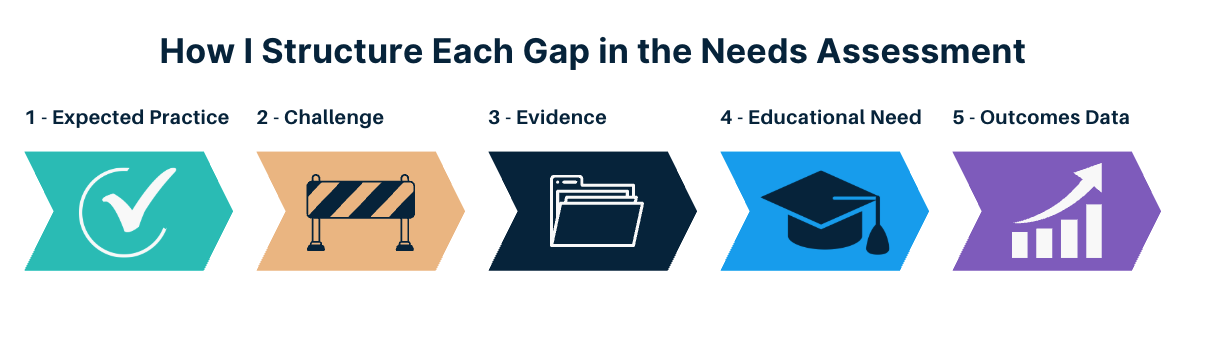
Not all evidence types are available for every gap, and this structure isn’t rigid, but it provides a narrative framework that allows me to shape a story that is clear, persuasive, and grounded in strategy.
Once the content is organized into this structure, I move into the drafting phase — not by writing linearly, but by working in bullets. This method allows me to quickly assemble, refine, and shape the narrative before committing to full paragraphs.
Here’s how it works:
- As I review my sources, I extract key points as bullets and assign them to specific sections of the needs assessment.
- I organize those bullets within the gap framework described above — so each section has material aligned with expected practice, challenges, evidence, and so on.
- When I am ready to write paragraphs, I polish each bullet into a sentence, then develop those sentences into full paragraphs.
- I also use reverse outlining to edit: if a paragraph feels off, I break it back into bullets to reassess flow, eliminate redundancies, or improve logic.
This method makes the writing more efficient and the final product more coherent. It also helps me catch inconsistencies or weak points early, saving time during revisions and ensuring each section builds a clear, evidence-based case for education.
By using a consistent structure for each gap and drafting with intention, I’m able to produce content that’s not just well-written, but strategically sound and easy to follow.
5. Designing the Educational Agenda
While drafting the educational agenda is the final step, I begin thinking about it from the very start of the project. Usually, clients come in with a proposed activity format. As I research and build the narrative, I keep this in mind, evaluating whether the proposed format aligns with the gaps and educational needs I am uncovering.
When it is time to write the agenda, I start with the client’s template but focus on translating the narrative into a program that:
- Addresses the identified gaps
- Matches the appropriate learning level
- Aligns with the client’s strategy and the sponsor’s educational guidelines
The agenda serves as a bridge between the proposal and the eventual activity. It is the roadmap for what comes next — and it needs to be as thoughtful as the needs assessment itself.
Conclusion
A strong needs assessment does not just describe the problem — it strategically defines it, supports it with evidence, and lays the groundwork for an effective educational intervention.
By following a clear, consistent process rooted in clinical insight, careful research, and thoughtful structure, I help clients move from an initial idea to a compelling proposal. Every needs assessment I write is designed to bring clarity, credibility, and direction. When the foundation is solid, the education that follows is stronger and the outcomes are more impactful for everyone involved.
Post a comment